How Cold Laser Treatment Helps Speed Up Healing After Injury
If you’re an athlete, a weekend warrior, or simply someone who has experienced an injury, the road to recovery can often feel long and frustrating. Whether it’s a sprained ankle, a nagging case of tendonitis, or a more serious muscle tear, the desire to get back to full function as quickly and safely as possible is universal. In the quest for faster healing, various therapies have emerged, and one that’s gaining significant traction in sports medicine, physical therapy, and rehabilitation circles is cold laser treatment.
Also known as low-level laser therapy (LLLT), cold laser treatment in Los Angeles is a non-invasive, drug-free, and painless approach that uses specific wavelengths of light to stimulate the body’s natural healing processes. It’s a promising option that claims to help reduce pain, decrease inflammation, and accelerate tissue repair.
But if you’re recovering from an injury, could light really help you heal faster? Let’s look at the science and practical applications of this innovative therapy.
What Is Cold Laser Treatment?
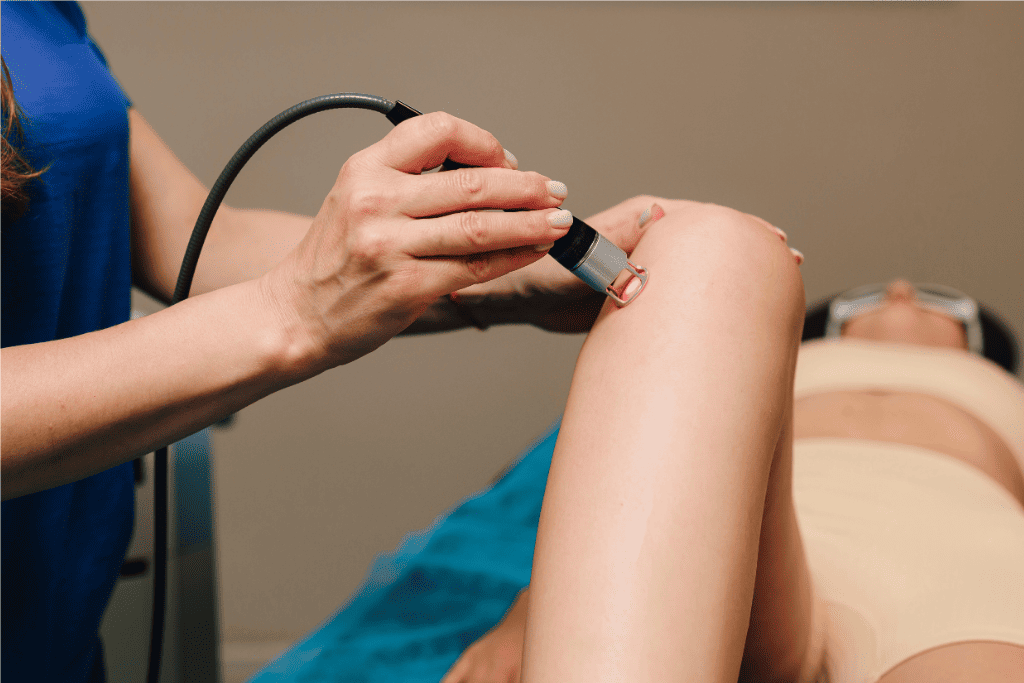
At its core, cold laser treatment involves the application of a low-power laser or LED light to an injured area of the body. Unlike the high-power lasers used in surgery that generate heat and cut tissue, cold lasers are “cold” because they don’t produce significant heat. Instead, they operate at much lower power levels, typically measured in milliwatts, and the light is absorbed by the cells without causing thermal damage.
The devices used in clinical practice are typically handheld probes that are placed directly on or near the skin over the injured area. These devices emit light in the red and near-infrared spectrum, which are wavelengths that have been shown to have therapeutic effects on biological tissues. Cold laser therapy is considered safe for treating a wide range of soft tissue and joint injuries.
The Science Behind Healing With Light
The fundamental principle behind cold laser therapy is photobiomodulation. This is a fancy term for how light energy penetrates the skin and interacts with the cells and tissues beneath. When the photons of light from the laser are absorbed by chromophores (light-sensitive molecules) within the cells, it triggers a cascade of cellular events.
One of the most significant cellular effects is the stimulation of mitochondria, often referred to as the “powerhouses” of the cell. This stimulation leads to an increase in the production of adenosine triphosphate (ATP), which is the primary energy currency of the cell. With more energy, cells can function more efficiently, leading to enhanced repair and regeneration processes.
Beyond increased ATP production, cold laser therapy has several other beneficial effects on the injured area:
- Improved Blood Flow: The light energy can help to dilate blood vessels, increasing circulation to the injured site. This delivers more oxygen and essential nutrients to the damaged tissues while also helping to remove waste products.
- Enhanced Collagen Production: Collagen is a vital protein that provides structural support to tissues. Cold laser therapy can stimulate fibroblasts, the cells responsible for producing collagen, thus aiding in the repair and strengthening of damaged tissues, including tendons, ligaments, and skin.
- Reduced Inflammation: The therapy can modulate the inflammatory response, decreasing the production of pro-inflammatory mediators and promoting the release of anti-inflammatory molecules. This helps to reduce swelling and pain, which are common companions to injury.
- Accelerated Lymphatic Drainage: By promoting lymphatic activity, cold laser therapy can help to clear away excess fluid and cellular debris from the injured area, further reducing swelling and contributing to faster healing.
- Pain Modulation (Analgesic Effect): Cold laser therapy can directly affect nerve cells, potentially reducing the excitability of pain nerves and stimulating the release of endorphins, the body’s natural painkillers.
Types of Injuries That Benefit From Cold Laser
Given its diverse cellular effects, cold laser therapy can be a valuable adjunct in the treatment of various injuries and conditions, including:
- Soft Tissue Injuries: This includes common ailments like sprains (ligament injuries), strains (muscle or tendon injuries), tendonitis (inflammation of tendons like Achilles tendonitis or tennis elbow), and fasciitis (inflammation of fascia, such as plantar fasciitis).
- Joint Injuries: Mild arthritis flare-ups, certain overuse injuries affecting joints, and conditions like bursitis can often benefit from the anti-inflammatory and pain-reducing effects of LLLT.
- Muscle Tears and Bruising: The therapy can aid in the repair of damaged muscle fibers and help resolve hematomas (bruises) more quickly by improving circulation and lymphatic drainage.
- Post-Surgical Wounds: Cold laser can be used to promote healing of surgical incisions and reduce scarring, contributing to a smoother recovery after operations.
- Chronic Injuries That Haven’t Fully Healed: For injuries that have lingered for an extended period, cold laser therapy can often provide the necessary cellular stimulation to kickstart or complete the healing process.
Benefits of Cold Laser Therapy for Healing
The advantages of incorporating cold laser therapy into an injury recovery plan are numerous:
- Faster Recovery Time: By accelerating cellular repair and reducing inflammation, cold laser therapy can significantly shorten the overall recovery period compared to relying solely on rest and time.
- Reduced Pain and Swelling: Patients often experience a noticeable decrease in pain and a reduction in swelling relatively quickly after starting treatment.
- Improved Range of Motion: By alleviating pain and inflammation and promoting tissue repair, cold laser therapy can help individuals regain their full range of motion more quickly during the recovery process.
- Non-Invasive and No Medications Required: This drug-free approach means no concerns about side effects commonly associated with pain medications or anti-inflammatory drugs.
- Minimal to No Side Effects: When administered properly by a trained professional, cold laser therapy is very safe, with minimal to no reported side effects. Patients typically feel nothing or a mild, soothing warmth during the treatment.
What to Expect During Treatment
A typical cold laser therapy session is quick and painless. The duration of a session can vary depending on the size of the area being treated and the specific condition, but it usually ranges from a few minutes to about 15-20 minutes. During the session, the practitioner will place the handheld laser device directly on your skin over the injured area. You won’t feel any heat or discomfort, though some people report a gentle tingling sensation.
The number of sessions required also varies, but it’s common for individuals to undergo a series of treatments, often 2-3 times per week initially, for several weeks. Many patients begin to notice improvement within a few sessions, with progressive benefits observed over the course of their treatment plan.
Cold laser therapy is often recommended as part of a comprehensive rehabilitation program, working synergistically with physical therapy exercises, manual therapy, and other modalities to optimize healing and recovery. Your healthcare provider or physical therapist will develop a personalized treatment plan tailored to your specific injury and recovery goals.
Conclusion
Cold laser therapy offers a compelling approach to accelerating the healing process after an injury. By harnessing the power of light, it effectively supports the body’s natural regenerative mechanisms, reducing pain and inflammation while enhancing cellular repair. Its non-invasive nature, lack of side effects, and impressive results make it an increasingly popular choice for athletes and individuals seeking a quicker return to their active lives.
If you’re struggling with an injury and looking for innovative ways to speed up your recovery, it’s worth talking to the experts at Urgent Orthopedic Care. They can assess your condition and determine whether cold laser therapy is the right option for you.